Labeling exercise 8-2 requisition and blood specimen label – Labeling Exercise 8-2: Requisition and Blood Specimen Label introduces the crucial practice of accurate labeling in healthcare, emphasizing its significance in ensuring patient safety and preventing medical errors. This comprehensive guide delves into the steps involved in completing the labeling exercise, highlights common pitfalls to avoid, and explores best practices for clear and legible labels.
Labeling Exercise 8-2 Requisition and Blood Specimen Label
Labeling Exercise 8-2 is a crucial step in ensuring the accuracy and safety of patient care. It involves the proper labeling of both the requisition form and the blood specimen itself. By completing this exercise, healthcare professionals can enhance their understanding of the labeling process and minimize the risk of errors.
Steps Involved in Completing Labeling Exercise 8-2, Labeling exercise 8-2 requisition and blood specimen label
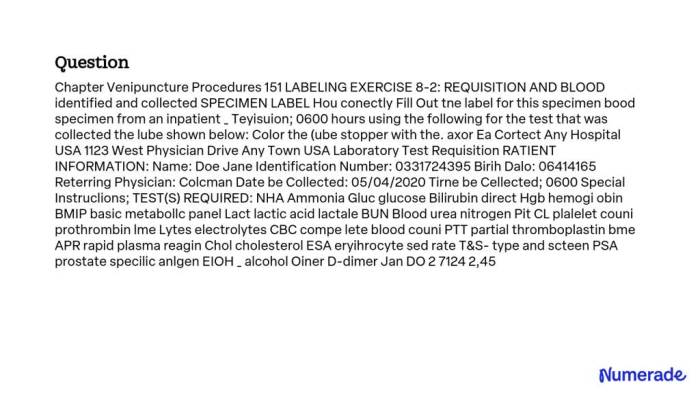
- Review the requisition form and ensure that all required information is present and accurate.
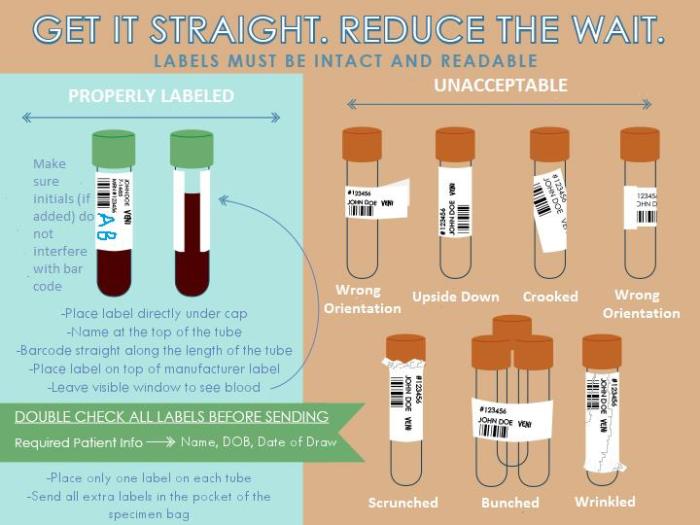
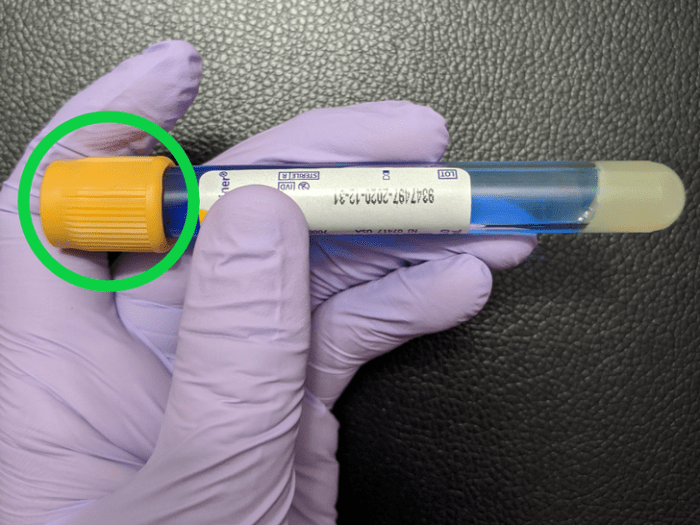
- Label the blood specimen tube with the patient’s name, date of birth, and the date and time of collection.
- Attach the labeled specimen tube to the requisition form.
- Verify the accuracy of the labels by comparing them to the requisition form.
- Document the labeling process in the patient’s medical record.
Common Errors in Labeling Exercise 8-2 and How to Avoid Them
- Incorrect patient information:Ensure that the patient’s name, date of birth, and other identifying information are accurate on both the requisition form and the blood specimen label.
- Incomplete information:Make sure that all required fields on the requisition form are completed, including the patient’s medical history, reason for testing, and any special instructions.
- Illegible handwriting:Write clearly and legibly on both the requisition form and the blood specimen label to avoid misinterpretation.
- Improper use of abbreviations:Use standardized abbreviations and avoid using ambiguous or uncommon terms.
Importance of Accurate Labeling
Accurate labeling is paramount in healthcare settings as it ensures patient safety and prevents medical errors. Mislabeling blood specimens can lead to incorrect diagnoses, inappropriate treatment, and even life-threatening consequences.
Potential Consequences of Mislabeling Blood Specimens:
- Delayed or incorrect treatment
- Transfusion of incompatible blood products
- Spread of infectious diseases
- Legal liability
Case Studies:
- A patient received the wrong blood transfusion due to a mislabeled specimen, resulting in a severe allergic reaction.
- A mislabeled specimen led to an incorrect diagnosis of leukemia, causing unnecessary anxiety and distress for the patient.
Best Practices for Labeling
To ensure clear and legible labels, follow these best practices:
Handwriting
- Write in block letters using a pen with dark ink.
- Avoid using cursive or script fonts.
- Print clearly and legibly, leaving no room for misinterpretation.
Abbreviations
- Use standardized abbreviations approved by the healthcare organization.
- Avoid using ambiguous or uncommon terms.
- Spell out abbreviations that may be unfamiliar to other healthcare professionals.
Adherence to Standardized Protocols
- Follow the established labeling protocols of the healthcare organization.
- Ensure that all required information is included on the label.
- Verify the accuracy of the label by comparing it to the requisition form.
Key Elements to Include on a Blood Specimen Label:
| Element | Description |
|---|---|
| Patient’s Name | Full name of the patient |
| Date of Birth | Patient’s date of birth |
| Date and Time of Collection | Date and time the specimen was collected |
| Specimen Type | Type of specimen collected (e.g., blood, urine) |
| Preservatives | Any preservatives added to the specimen |
Quality Control Measures
To prevent labeling errors, it is crucial to implement quality control measures.
Methods of Quality Control:
- Double-Checking:Two healthcare professionals independently verify the accuracy of the labels.
- Electronic Verification:Using electronic systems to scan and compare labels to the requisition form.
- Audits:Regular reviews of labeling practices to identify and address potential errors.
Benefits of Quality Control Measures:
- Reduces the risk of labeling errors
- Improves patient safety
- Enhances confidence in the accuracy of laboratory results
Technology and Automation: Labeling Exercise 8-2 Requisition And Blood Specimen Label
Technology and automation can play a significant role in improving the efficiency and accuracy of labeling processes.
Benefits of Automated Labeling Systems:
- Reduced human error
- Increased efficiency and speed
- Improved legibility and standardization
Case Study:
- A hospital implemented an automated labeling system, which reduced labeling errors by 75% and improved turnaround time for laboratory results.
Helpful Answers
What is the purpose of Labeling Exercise 8-2?
Labeling Exercise 8-2 aims to reinforce the importance of accurate labeling in healthcare, particularly in the context of requisition and blood specimen labels.
What are some common errors made during Labeling Exercise 8-2?
Common errors include illegible handwriting, incorrect patient information, and omission of essential details.
How can quality control measures help prevent labeling errors?
Quality control measures, such as double-checking and electronic verification, provide an additional layer of scrutiny to ensure the accuracy of labels.